Colonoscopy
WHAT IS A COLONOSCOPY?
This procedure involves a colonoscope – a long, thin flexible tube with a ‘video camera’ at the tip – being passed through the rectum into the colon. It allows the doctor to inspect the large intestine and also perform specialised procedures such as biopsies and removal of polyps.
WHY HAVE A COLONOSCOPY?
A colonoscopy can detect inflamed tissue, ulcers and abnormal growths. The procedure is used to look for early signs of colorectal cancer and can help doctors diagnose unexplained changes in bowel habits, abdominal pain, bleeding from the bowel and weight loss. In some individuals with a family history, this may also be an appropriate test to check for bowel cancer.
HOW DO I PREPARE FOR A COLONOSCOPY?
For a successful colonoscopy, it is essential to empty the bowel thoroughly of all waste material, which can be done by taking a bowel preparation (see below). Failure to do this prior to colonoscopy may mean the doctor won’t be able to see important markers, or you may have to return for another procedure.
A complete bowel preparation consists of:
- Modifying your diet
This may involve following a special diet for several days prior to the colonoscopy.
- Taking a bowel preparation medication
There are several effective bowel preparations (laxative medication that causes diarrhoea and empties the colon) available and, depending on your medical condition, the doctor will recommend the right one for you.
- Increasing your fluid intake
Specific preparation instructions will be given to you by your doctor.
Patients should also inform the doctor of all medical conditions and any medications, vitamins or supplements taken regularly.
HOW IS A COLONOSCOPY PERFORMED?
Sedation
Before the procedure a light anaesthetic (sedative) is usually given – you will not receive a full general anaesthetic. You may be slightly aware of what is going on in the room, but generally you won’t remember anything. The doctor and medical staff monitor your vital signs during the procedure and will attempt to make you as comfortable as possible.
A colonoscopy usually takes between 20 and 45 minutes.
Examination of the bowel
Once sedated and lying in a comfortable position on your left side, the doctor inserts the flexible colonoscope (‘scope’) through the anus and slowly guides it into the colon. A small camera in the end of the scope transmits a video image to a monitor, allowing the doctor to carefully examine the intestinal lining.
Once the scope has reached the opening to the small intestine, it is slowly withdrawn and the lining of the large intestine is carefully examined again.
Removal of polyps and biopsy
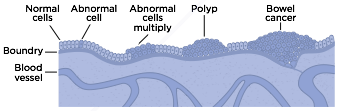
A polyp is a small tissue growth attached to the bowel wall. These are common in adults and are usually harmless, however, most colorectal cancer begins as a polyp so removing them early is an effective way to prevent cancer.
If polyps are found during the procedure they will usually be removed using tiny tools passed through the scope. Small tissue samples or biopsies of the bowel may also be taken for examination. This allows the doctor to review it with a microscope for signs of disease.
The Beginnings of Bowel Cancer
WHAT HAPPENS AFTER A COLONOSCOPY?
Following the procedure you will remain in the recovery area for an hour or two until the sedation medication wears off. You will usually be given something light to eat and drink once you are awake.
When you wake up you may feel a little bloated. This is due to the air that was inserted during the procedure, and will pass over the next hour or so.
Very rarely you may pass a small amount of blood. This is often due to biopsies that have been taken and shouldn’t concern you.

A complete bowel preparation is essential for an accurate and safe colonoscopy. Please follow the bowel preparation instructions carefully.
Because of the sedation given during the procedure, it is very important that you do not drive a car, travel on public transport alone, operate machinery, sign legal documents or drink alcohol on the same day after the test. It is strongly advice that a friend or relative take you home and stay with you.
Full recovery is expected by the next day. Discharge instructions should be carefully read and followed.
ARE THERE ANY RISKS OR SIDE-EFFECTS?
Although complications can occur, they are rare when the procedure is performed by doctors who are specially trained to perform a colonoscopy.
In Australia, very few people experience serious side-effects from a colonoscopy and polypectomy (polyp removal).
The chance of complications depends on the exact type of procedure that is being performed and other factors including your general health.
After the procedure you may feel bloated, and if a biopsy has been taken or treatment performed there may be minor bleeding. Very rarely (one in 1,000 cases), the bowel lining may be torn, and if this occurs you will be admitted to hospital for an operation to repair it.
Occasionally, people may be intolerant to the bowel preparation medication and experience headaches or vomiting.
Reactions to the sedative are also possible, but again rare.
In a few cases, if the colonoscopy is not successfully completed it may need to be repeated.
If you have any of the following symptoms in the hours or days after the colonoscopy you should contact the hospital or your doctor’s rooms immediately:
- Severe abdominal pain
- Black, tarry motions
- Persistent bleeding from the anus
- Fever
- Other symptoms that cause you concern
HOW ACCURATE IS A COLONOSCOPY?
A colonoscopy is considered to provide the most accurate assessment of the colon. However, no test is perfect and there is a risk that an abnormality may not be detected.
A colonoscopy can miss lesions in the bowel in 2% – 8% of cases. For serious lesions such as cancer, the chance is much less, but still present. For these reasons, it is recommended that all patients over the age of 50, and those with a family history of colorectal cancer, perform a faecal occult blood (FOB) test every one to two years. The test kits are available from your chemist or local doctor.
STERILISATION OF THE INSTRUMENTS
In accordance with GESA guidelines, the colonoscope should be completely cleaned and all instruments sterilised between each patient so that there is no risk of transmission of serious diseases such as HIV and Hepatitis B or C.
WHO CAN I CONTACT IF I HAVE ANY QUESTIONS?
If you have any questions or need advice, please contact us here at Gippsland Gastroenterology.
TAKE HOME POINTS
- Colonoscopy is a procedure used to see inside the colon and rectum.
- Prior to the procedure, use a bowel preparation kit to empty all solids from the gastrointestinal tract. Read the instructions carefully.
- During the colonoscopy a light anaesthetic is often used to keep the patient comfortable.
- The doctor will usually remove polyps and biopsy abnormal-looking tissue during the colonoscopy.
- Driving is not permitted for 24 hours after gastroscopy to allow the sedative time to wear off.
Digestive Health Foundation Disclaimer
This information leaflet has been designed by the Digestive Health Foundation (DHF) as an aid to people who will undergo gastroscopy or for those who wish to know more about it. This is not meant to replace personal advice from your medical practitioner.
The DHF is an educational body committed to promoting better health for all Australians by promoting education and community health programs related to the digestive system.
The DHF is the educational arm of the Gastroenterological Society of Australia (GESA), the professional body representing the specialty of gastrointestinal and liver disease. Members of the Society are drawn from physicians, surgeons, scientists and other medical specialties with an interest in gastrointestinal (GI) disorders. GI disorders are the most common health-related problems affecting the community.
Research and education into gastrointestinal disease are essential to contain the effects of these disorders on all Australians.
Further information on a wide variety of gastrointestinal conditions is available on the Gastroenterological Society of Australia website.