Coeliac Disease
What is Coeliac disease?
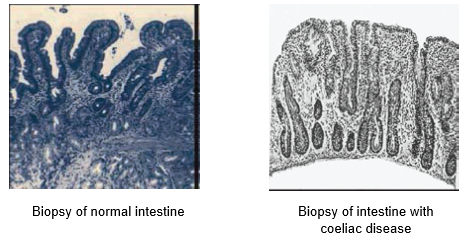
Coeliac disease is an autoimmune disorder which results in damage to the small intestine lining (villi) when exposed to gluten, the protein component found in wheat, barley, rye and oats. Villi are tiny hair-like structures on the lining of the small intestine that absorb nutrients from food.
How does it affect the body?
When someone with coeliac disease consumes gluten, their immune system forms antibodies in response. These antibodies then attack the intestinal lining and cause inflammation and damage to the villi. If the villi are inflamed, it is difficult for the body to absorb nutrients properly which can lead to nutrient malabsorption and deficiencies.
How common is coeliac disease?
Coeliac disease can present at any age, although it more commonly presents in childhood. It affects 1 in 60 women and 1 in 80 men in Australia and occurs in 10% of first-degree relatives.
The HLA DQ2 and HLA DQ8 genes are associated with the development of coeliac disease. Approximately 30% of the population carry one or both of these genes, however only 1 in 30 people will develop coeliac disease.
Presentation
The symptoms of coeliac disease can range from severe, minor or may go undetected. Symptoms can be confused with irritable bowel syndrome (IBS). It is strongly recommended if you suffer from IBS-like symptoms that you are investigated for coeliac disease.
- Gastrointestinal issues
- Diarrhoea
- Constipation
- Flatulence
- Bloating
- Nausea
- Abdominal pain
- Lethargy
- Poor weight and growth in children
- Vitamin and mineral deficiencies (specifically iron, folate, zinc, Vitamin D)
- Osteopaenia and osteoporosis
- Delayed periods
- Infertility (in both males & females)
- Mouth ulcers
Methods of diagnosis
Initially, the doctor may screen you for coeliac disease by doing a blood test (coeliac serology and IgA). If the test result is positive, you may be referred to a gastroenterologist to confirm the diagnosis with a small bowel biopsy.
To conduct the biopsy, a gastroscopy is performed under sedation. The gastroenterologist takes a tiny sample of your small intestine and examines it under a microscope for signs of inflammation. This method of diagnosis requires the consumption of gluten at least 2 weeks prior to investigation.
Why?
Correct diagnosis of coeliac disease can only be made if the lining of the intestine is damaged. Going on a gluten-free diet prior to the investigation can lead to a false negative diagnosis.
Treatment
The only treatment for coeliac disease is a life-long gluten-free diet. A gluten-free diet will prevent further damage to the lining of the intestine, and allow for the villi to heal so that nutrients from food can be absorbed. The diet is strict, as even a small amount of gluten-containing food like pasta or bread can cause inflammation.
Ongoing monitoring is important to ensure the intestinal lining is healing and the villi are growing back.
How can a dietitian help?
As the gluten-free diet is life-long and strict, dietary compliance is imperative. A dietitian can provide you with strategies to facilitate the gluten-free diet into your life. You will be educated on label reading, sneaky gluten-containing food products and even what questions to ask when you’re out for a meal!
Although it will feel challenging during the initial months post diagnosis, the gluten-free diet will become easier over time as you become familiar with label reading and food products containing gluten.
Sources